Cancers, Vol. 13, Pages 2100: BLBP Is Both a Marker for Poor Prognosis and a Potential Therapeutic Target in Paediatric Ependymoma
Cancers doi: 10.3390/cancers13092100
Authors: Durgagauri H. Sabnis Jo-Fen Liu Lucy Simmonds Sophie Blackburn Richard G. Grundy Ian D. Kerr Beth Coyle
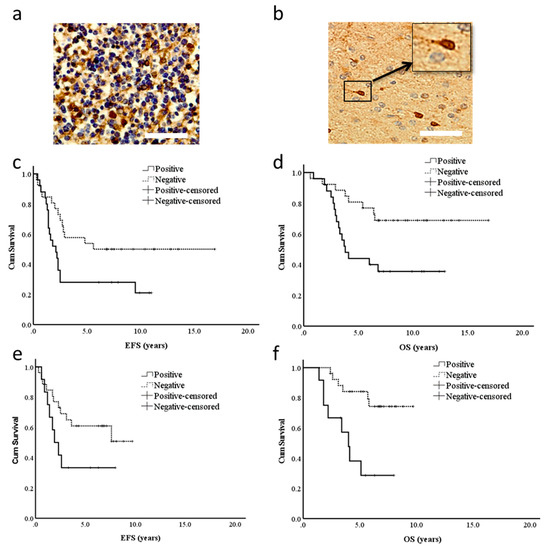
Paediatric ependymomas are aggressive, treatment-resistant tumours with a tendency towards relapse, consistent with a sub-population of therapy-resistant cancer stem cells. These cells are believed to derive from brain lipid binding protein (BLBP)-expressing radial glia, hence we proposed that BLBP may be a marker for ependymoma therapy resistance. BLBP protein expression correlated with reduced overall survival (OS) in patients from two trials (CNS9204, a chemotherapy-led infant trial—5 y OS 45% vs. 80%, p = 0.011—and CNS9904, a radiotherapy-led trial—OS 38% vs. 85%, p = 0.002). All ependymoma cell lines examined by qRT-PCR expressed BLBP, with expression elevated in stem cell-enriched neurospheres. Modulation of BLBP function in 2D and 3D assays, using either peroxisome proliferator activated receptor (PPAR) antagonists or BLBP's fatty acid substrate docosahexaneoic acid (DHA), potentiated chemotherapy response and reduced cell migration and invasion in ependymoma cell lines. BLBP is therefore an independent predictor of poor survival in paediatric ependymoma, and treatment with PPAR antagonists or DHA may represent effective novel therapies, preventing chemotherapy resistance and invasion in paediatric ependymoma patients.