Successful treatment of pyopneumothorax secondary to Streptococcus constellatus infection with linezolid: a case report and review of the literature:
Abstract
Background
Pyopneumothorax secondary to Streptococcus constellatus infection is a clinically rare event, and few cases have been reported.
Case presentation
We report the case of a 55-year-old Han Chinese man with underlying diabetes who presented with fever of 17 days duration. A pulmonary computed tomography scan revealed right-sided massive pyopneumothorax. A culture of the pleural effusion and blood grew S. constellatus. A drug sensitivity test showed that the isolate was sensitive to linezolid, penicillin G, cefotaxime, vancomycin, and cefuroxime. Our patient was treated with linezolid for a total of 6 weeks. Subsequently, his chest computed tomography scan showed improved lung condition.
Conclusion
To the best of our knowledge, this is the first case of pyopneumothorax secondary to S. constellatus to be treated with linezolid. Pyopneumothorax may be caused by streptococcal infection, and linezolid is another good choice for treatment.
Peer Review reports
Background
Streptococcus constellatus belongs to the Streptococcus milleri group of bacteria, which consists of S. constellatus, Streptococcus intermedius, and Streptococcus anginosus [1]. S. constellatus usually causes abscesses in various organs. Linezolid has not been reported to treat pyopneumothorax caused by S. constellatus infection. Here, we report a case of successful treatment of a patient with pyopneumothorax due to S. constellatus infection. This case contributes valuable information to the current knowledge on the treatment of this infectious disease.
Case presentation
A 55-year-old Han Chinese man was admitted to our hospital on July 26, 2018 on presenting with a chief complaint of fever. Our patient began to have fever 17 days prior to his presentation, and his highest temperature had been 38.5 °C, accompanied by pain in his right chest and cough. He denied symptoms of chest tightness, nausea, and vomiting. He had taken oral amoxicillin without obvious effect, and the symptoms of fever and chest pain continued. He denied hepatitis, tuberculosis, and a history of hypertension or diabetes mellitus.
On admission, a physical examination revealed a temperature of 36.5 °C and blood pressure of 115/70 mmHg with a pulse rate of 75 beats per minute (bpm). A lung examination revealed reduced breath sound in the right lung field. The breath sound in the left lung was clear. A lung computed tomography (CT) scan (July 26, 2018) showed pyopneumothorax of the right lung and lower lobe right lung infection (Fig. 1); a cardiac ultrasound was normal.
Fig. 1
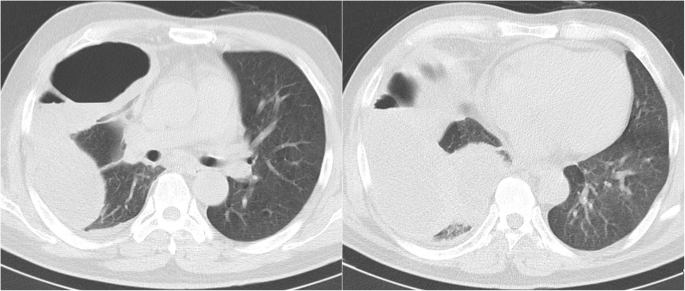
Chest computed tomography scan revealing right-sided massive pleural effusion with pneumothorax. Date: July 26, 2018
Full size image
Investigation
Routine blood workup (July 26, 2018) results showed his WBC count was 19.24 × 109/l(4–10 × 109/l), neutrophils were 87.1% (50–70%), C-reactive protein was 10.6 mg/dl (0–0.8 mg/dl), serum albumin was 27.3 g/l (35–55 g/l), and his blood glucose was 11.06 mmol/l (3.9–6.1 mmol/l). Hepatitis B antigen and human immunodeficiency virus (HIV) antigen test results were all negative. His procalcitonin was 0.606 ng/ml (< 0.05 ng/ml), and glycosylated hemoglobin was 6.8% (4–6%). The initial diagnoses of our patient were pyopneumothorax, hypoalbuminemia, and type 2 diabetes. According to the local epidemiologic characteristics, differential diagnosis included lung abscess, community-acquired pneumonia, and pulmonary tuberculosis.
Treatment
Our patient was initially treated with closed chest drainage, and there was persistent drainage of pus from his right chest. He was treated with imipenem, linezolid to control the infection, and insulin to control his blood glucose. Pleural fluid culture and blood culture grew S. constellatus, which was sensitive to linezolid, penicillin G, cefotaxime, vancomycin, and cefuroxime. The drug susceptibility test is shown in Table 1. On October 8, 2018, the antibiotic regimen was changed to intravenous linezolid. There were no adverse or unanticipated events for linezolid treatment. On October 11, 2018, a chest CT scan (Fig. 2) showed reduced pleural effusion and pulmonary infection of the right lung. On October 24, 2018, the drainage tube was removed.
Table 1 Drug sensitivity to Streptococcus milleri
Full size table
Fig. 2
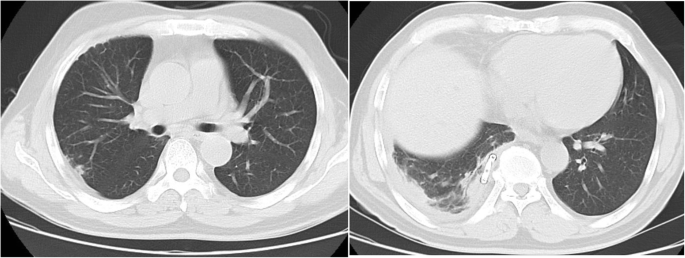
Chest computed tomography scan revealing right-sided pleural effusion and pulmonary infection. Date: October 11, 2018
Full size image
Outcome and follow-up
Our patient was discharged with oral linezolid treatment for 1 week. He was prescribed a total of 6 weeks of linezolid treatment, including 5 weeks of intravenous linezolid and 1 week of oral linezolid treatment. A subsequent follow-up chest CT scan (Fig. 3) showed mass absorption of pyopneumothorax and pulmonary infection.
Fig. 3
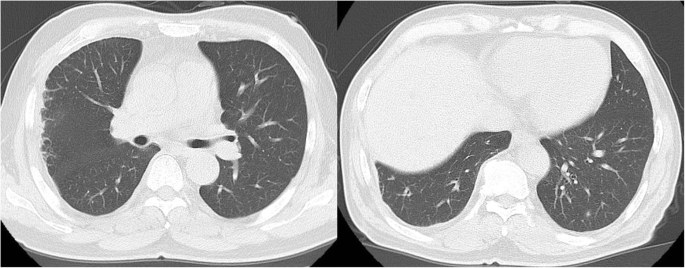
Chest computed tomography scan revealing slight right-sided pleural effusion and pulmonary infection. Date: November 16, 2018
Full size image
Discussion and conclusion
Pyopneumothorax is the accumulation of gas and pus in the pleural cavity. Bacteria that frequently cause pyopneumothorax include Pseudomonas aeruginosa, Escherichia coli and Streptococcus [2].
The S. milleri group is a heterogeneous group of Streptococci, which is considered an important pathogen. It consists of three distinct species: S. anginosis, S. constellatus and S. intermedius. S. milleri has emerged in recent years as an organism associated with purulent disease in humans. S. constellatus is usually present in the normal flora of the mouth, vagina, respiratory tract, and gastrointestinal tract [3, 4]. Distinct species have been implicated in a number of pyogenic infections, including soft tissue infection, intra-abdominal and pulmonary abscesses, and central nervous system infections [5]. There is a considerable mortality rate from S. milleri infection. Fernando Cobo reported that the mean age at diagnosis was 62.06 ± 15 years. Two of 12 patients with S. milleri infection died as a consequence of infection. Risk factors for S. milleri infection include alcoholism, chronic obstructive pulmonary disease, and diabetes mellitus. The most frequently used antimicrobials for treatment were ceftriaxone and levofloxacin [5].
Cases of pyopneumothorax secondary to S. milleri infection have rarely been reported [6, 7]. Our case is the third case report of patients with pyopneumothorax caused by S. milleri. The summarization of the three cases are shown in Table 2. The first case was a 37-year-old man with hepatitis C infection. A chest radiograph and CT scan showed a large pleural cavity in the right hemithorax with an air-fluid level. The patient received empiric antibiotic therapy with cefuroxime and clindamycin. The patient recovered upon antibiotic treatment and drainage and was dismissed from the hospital after 17 days to home care [7]. The second patient was a 46-year-old Malay woman with underlying hypothyroidism post thyroidectomy who presented with worsening breathlessness, orthopnea, productive cough, and left-sided pleural chest pain of 3 days’ duration. The patient was treated with antibiotics for a total of 6 weeks and underwent open thoracotomy and decortication during admission [6]. In the current case, infection occurred primarily without any pre-existing pulmonary sequence or long treatment history. The patient was apparently healthy without any history of immunosuppression. However, her blood glucose was higher than normal, and diabetes was diagnosed on admission. The patient had undiagnosed type 2 diabetes before admission to our hospital. A previous study showed that diabetes is a risk factor for S. milleri group infection [5]; therefore, we deduced that the infection might have been related to the rise of blood glucose.
Table 2 Summarization of the three cases
Full size table
In our case, we did not use cefuroxime and clindamycin as the empirical treatment. A drug sensitivity test showed that S. milleri was sensitive to linezolid, penicillin G, cefotaxime, vancomycin, and cefuroxime. Linezolid can be considered as the first member of the class of oxazolidinone antibiotics. Linezolid has been approved by the Food and Drug Administration for the treatment of the following: Staphylococcus aureus, Streptococcus pneumonia, and vancomycin-resistant Enterococcus faecium (VREF) infections [8]. A previous study also showed that S. constellatus isolated from liver abscesses was also sensitive to linezolid; however, the patient was treated with ceftriaxone [9]. The main side effects of linezolid were hematologic side effects including myelosuppression and thrombocytopenia. The ordinary dose of linezolid was 0.6 g per 12 hours. We had to monitor the blood routine for side effects. Our patient did not show any hematologic side effects and his platelet count was in the normal range.
Our case showed successful treatment of pyopneumothorax secondary to S. constellatus with linezolid for 6 weeks. Our case indicated that pyopneumothorax may be caused by streptococcal infection and that linezolid is a good choice for treatment.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
bpm:
Beats per minuteHIV:
Human immunodeficiency virusVREF:
Vancomycin-resistant Enterococcus faeciumWBC:
White blood cell count
References
1.
Whiley RA, Beighton D. Emended descriptions and recognition of Streptococcus constellatus, Streptococcus intermedius, and Streptococcus anginosus as distinct species. Int J Syst Bacteriol. 1991;41(1):1–5.
CAS Article Google Scholar
2.
Ofosu AA. Diagnosis and treatment of pyopneumothorax. Trop Dr. 1997;27(4):252.
CAS Article Google Scholar
3.
Kim SH, Park MS, Song SH, Lee HJ, Choi EH. Hematogenous osteomyelitis caused by Streptococcus anginosus group in a previously healthy child. Pediatr Int. 2010;52(4):e209–11.
Article Google Scholar
4.
Sunwoo BY, Miller WT. Streptococcus anginosus infections: crossing tissue planes. Chest. 2014;146(4):e121–121e125.
Article Google Scholar
5.
Belko J, Goldmann DA, Macone A, Zaidi AK. Clinically significant infections with organisms of the Streptococcus milleri group. Pediatr Infect Dis J. 2002;21(8):715–23.
Article Google Scholar
6.
Che Rahim MJ, Mohammad N, Wan Ghazali WS. Pyopneumothorax secondary to Streptococcus milleri infection. BMJ Case Rep. 2016;2016:bcr2016217537.
Article Google Scholar
7.
Eller P, Theurl I, Koppelstaetter F, Weiss G. Pyopneumothorax due to Streptococcus milleri. Wien Klin Wochenschr. 2006;118(7–8):207.
Article Google Scholar
8.
SMR H, Farhadi T, Ganjparvar M. Linezolid: a review of its properties, function, and use in critical care. Drug Des Devel Ther. 2018;12:1759–67.
Article Google Scholar
9.
Mohanty S, Panigrahi MK, Turuk J, Dhal S. Liver abscess due to Streptococcus constellatus in an immunocompetent adult: a less known entity. J Natl Med Assoc. 2018;110(6):591–5.
Article Google Scholar
Download references
Acknowledgements
Not applicable.
Funding
The authors declare that no funding was received for this study.
Author information
Affiliations
Department of Respiratory Medicine, Chinese PLA General Hospital, 28 Fuxing Road, Haidian District, Beijing City, 100853, People’s Republic of China
Zhaorui Zhang, Binbin Xiao & Zhixin Liang
Contributions
ZZ and BX contributed to treatment decisions, data collection, and data analysis. ZZ and ZL contributed to writing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Zhixin Liang.
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review from the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and Permissions
About this article
Cite this article
Zhang, Z., Xiao, B. & Liang, Z. Successful treatment of pyopneumothorax secondary to Streptococcus constellatus infection with linezolid: a case report and review of the literature. J Med Case Reports 14, 180 (2020). https://doi.org/10.1186/s13256-020-02475-w
Download citation
Received25 April 2020
Accepted28 July 2020
Published07 October 2020
DOIhttps://doi.org/10.1186/s13256-020-02475-w
Share this article
Anyone you share the following link with will be able to read this content:Get shareable link
Provided by the Springer Nature SharedIt content-sharing initiative
Keywords
Pyopneumothorax
Streptococcus constellatus
linezolid
case report
Streptococcus milleri
treatment

Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου